

Diarrhoea






Diarrhoea
Diarrhoea can lead to dehydration and weight loss if left untreated.
What is diarrhoea? 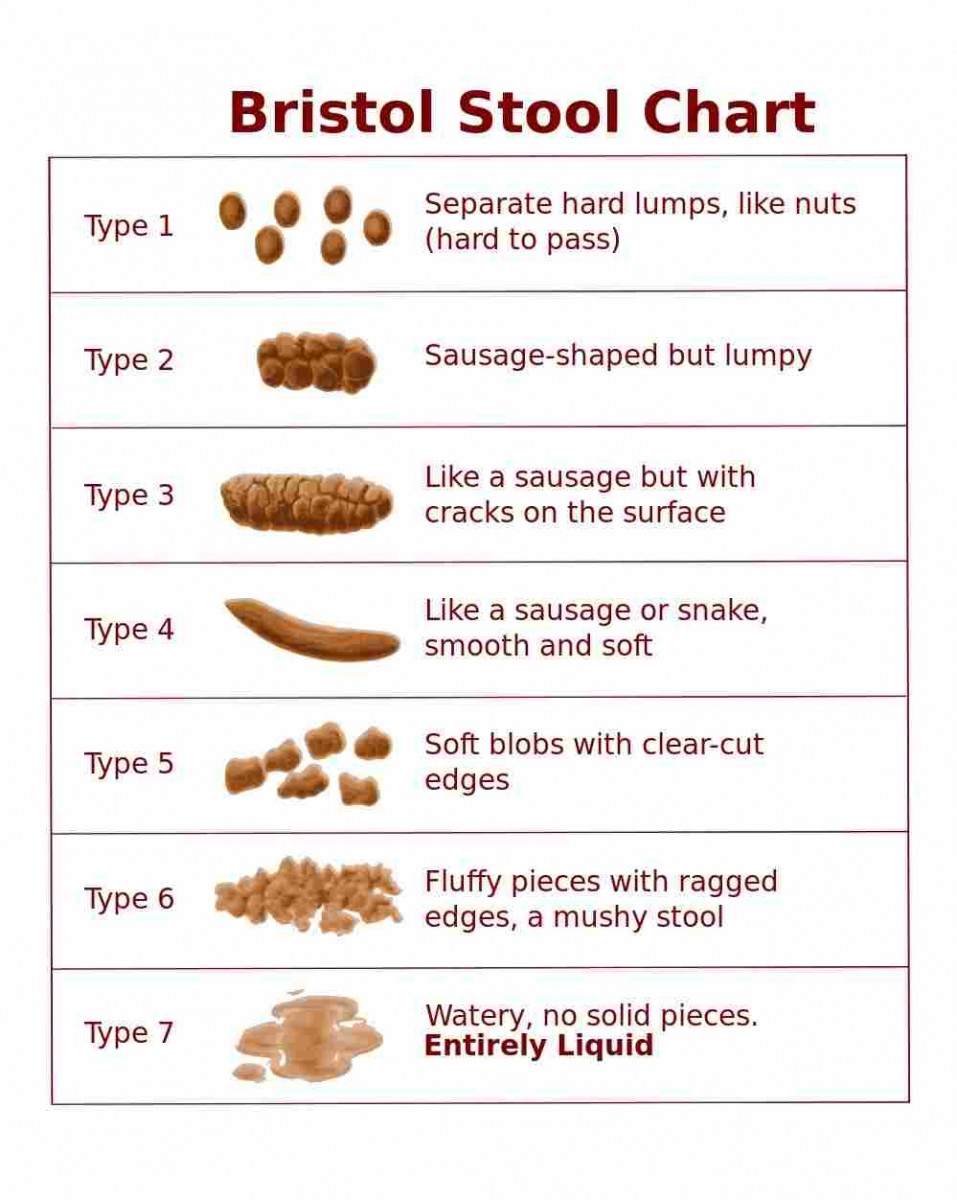
Diarrhoea is the passage of three or more loose or liquid stools a day or more than your normal. The Bristol Stool Chart is a recognised pictorial diagram used in healthcare that you can use to classify your stools. Type 5, type 6 and type 7 may indicate diarrhoea.
Why might I be having diarrhoea?
There are many reasons why you may have diarrhoea. The management and treatment of it usually depends on the cause. It is therefore useful to know the reason for your diarrhoea.
Diarrhoea can occur due to the cancer itself or as a result of damage or irritation to the digestive tract caused by some cancer treatments. Other reasons include;
- Side effects of medication i.e. antibiotics, laxatives
- Constipation overflow
- Infection
- Malabsorption
You may be asked to provide a stool sample to check for any infection.
How can I manage Diarrhoea?
In addition to medication, changes to what you eat and drink can help.
Keep yourself hydrated
 Although you may not feel like eating it is important that you do continue to eat and drink to keep yourself nourished and hydrated. Your body will lose a lot of water and salts if you have diarrhoea and you may be at risk of becoming dehydrated.
Although you may not feel like eating it is important that you do continue to eat and drink to keep yourself nourished and hydrated. Your body will lose a lot of water and salts if you have diarrhoea and you may be at risk of becoming dehydrated.
It can help to include drinks other than water to replace the salts. Tea, coffee, milk, water, fruit juice, soda, diluting juice, beef stock all count towards your body's fluid intake.
Sip fluid throughout the day and if you are going out take a drink with you.
Avoid known Irritants
These are food and drinks that are known to irritate the digestive tract. These can make your symptoms worse.
Alcohol |
If you drink alcohol you can find more information here about the low risk drinking guidelines and help to cut down how much you drink |
Smoking |
If you smoke, help to stop can be found here |
Carbonated drinks |
|
Spices or spicy food |
|
Caffeine |
|
Sorbitol |
|
Keep a food and symptom diary
 This can help to identify food and drinks that are troublesome for you. You may wish to avoid these foods to see if this helps. If you don’t notice an improvement with avoiding certain food and drinks try reintroducing these back in to your diet. It is important to have a varied diet to make sure you get everything you need. Avoiding certain food and drinks long-term unnecessarily is not recommended.
This can help to identify food and drinks that are troublesome for you. You may wish to avoid these foods to see if this helps. If you don’t notice an improvement with avoiding certain food and drinks try reintroducing these back in to your diet. It is important to have a varied diet to make sure you get everything you need. Avoiding certain food and drinks long-term unnecessarily is not recommended.
You can find details on a balanced diet here.
What about fibre?
 As part of a healthy balanced diet the general population is encouraged to eat 30g fibre per day. This can be difficult to achieve particularly if you have a poor appetite.
As part of a healthy balanced diet the general population is encouraged to eat 30g fibre per day. This can be difficult to achieve particularly if you have a poor appetite.
If you are adding fibre to your diet do it gradually introducing 1-2 changes every few days. This will help your bowel adjust and avoid bloating and excess gas.
For more information on how to include fibre in your diet visit The British Dietetic Association or British Nutrition Foundation.
Some people find reducing the fibre content of their diet when they have symptoms of diarrhoea can help. As a starting point see below for examples of higher and lower fibre containing foods.
Higher fibre alternative |
Lower fibre alternative |
| Seeded or wholemeal bread or bread products, pitta, wraps | White bread, white roll, white pitta bread, white wrap, crumpet, pancake |
| Oatcakes, Ryvita, flapjack | Cream crackers, breadsticks, rice cakes |
| Bran flakes, porridge oats, muesli, wholegrain cereal | Refined breakfast cereals i.e. corn or rice based cereal |
| Brown rice | White rice, basmati rice, noodles |
| Wholemeal pasta, quinoa | White pasta |
| Baked potato or boiled potato (with skin on), sweet potato or yam | Mashed or boiled potato or baked potato (without skin) |
| Nuts, seeds | Ground nuts |
| Lentils, kidney beans, yellow-split peas, baked beans, chickpeas | Skinned chicken, white fish, hard-boiled egg, scrambled egg |
| Fruit juice (with pulp/with bits) | Fruit juice (without pulp/without bits), diluting juice |
| Dried apricots, raisins, prunes | Peeled, skinless or tinned fruit i.e. apple, peach, pear |
| Orange, satsuma, apple (with skin), pear (with skin), kiwi fruit with seeds, watermelon, pineapple | Skinless or tinned fruit i.e. apple, peach, pear, ripe galia melon, banana. Avoid orange piths. |
| Peas, sweetcorn, raw vegetables i.e. carrot and salad vegetables including cucumber, lettuce, tomato | Well-cooked fruit and vegetables i.e. carrot, broccoli or grated vegetables |
What about fat?
A diet high in fat can contribute to diarrhoea. It may be worth considering reducing your intake or avoiding the following obvious sources of high-fat foods in the short-term:
- Batter
- Pastries
- Fried foods i.e. bacon, egg, sausages
- Take-aways
- Oily curries
Pancreatic exocrine insufficiency (PEI) can lead to malabsorption of fat and result in diarrhoea. There are effective treatments for this if this is the reason for your diarrhoea. Please discuss this with a healthcare professional for more information.
Following a 'low-fat' diet without medical reason is not recommended when you have cancer. This can accelerate weight loss and mean that you miss out on vital nutrients. Click here for more information on a healthy balanced diet.
What about lactose?
Chemotherapy damages healthy gut cells. Lactose intolerance can occur as a result of chemotherapy treatment. This normally resolves when you stop chemotherapy treatment.
Following a lactose free diet during your treatment can help. If you choose to follow a lactose-free diet for the duration of your treatment please read the advice here to make sure you are taking in enough calcium.
If you are having radiotherapy treatment, the evidence does not support following a lactose-free diet unless you have been diagnosed with lactose intolerance.
What about probiotics?
Taking probiotics is not recommended for someone with cancer.
Cancer and cancer treatment can reduce your ability to fight infection. Probiotics contain live bacteria and so consuming probiotics with having a weakened immune system can increase your risk of developing an infection.
Probiotics have in some cases been found to limit the length of time you have diarrhoea for and there is evidence to support their use in those with irritable bowel syndrome however taking probiotics is not recommended for someone with cancer. To find out more about probiotics check out the British Dietetic Association fact sheet on Probiotics.
What if I have had radiotherapy to my pelvic area?
If you have diarrhoea as a result of radiotherapy treatment the evidence no longer suggests that restricting your fibre intake will help.
Continue to eat as you usually would do. If you have diarrhoea consider your fluid intake, avoid known irritants and take your medication as prescribed. If your symptoms continue discuss changes to your medication with your healthcare team. An antispasmodic medication could help.
If your symptoms continue consider asking for a referral to a dietitian.
What if I have diarrhoea related to immunotherapy?
If you have diarrhoea as a result of immunotherapy treatment you are recommended to follow the advice above. This includes;
- Keep yourself hydrated
- Avoid food and drinks that are known to irritate the gut (irritants)
- Discuss uncontrolled symptoms and medication with your healthcare team
If your diarrhoea is associated with colitis your healthcare team will manage this. You may also benefit from a referral to a dietitian.
What if I have a stoma?
T he information on this page is not suitable for you if you have a stoma. Speak to your healthcare team if you are looking for advice specific to eating and drinking with a stoma.
he information on this page is not suitable for you if you have a stoma. Speak to your healthcare team if you are looking for advice specific to eating and drinking with a stoma.
What about medication?
 Continue to take any medication as prescribed, even if you think these are contributing to your loose stools, for example, antibiotics.
Continue to take any medication as prescribed, even if you think these are contributing to your loose stools, for example, antibiotics.
Anti-diarrhoeal medication can help your symptoms. Speak to your healthcare team if you do not have medication to help your symptoms, to discuss changes to current medications or if your symptoms persist despite medication.
