

Constipation






Constipation
Constipation can be unpleasant. It can make you feel generally unwell, full up and less hungry.
What is constipation?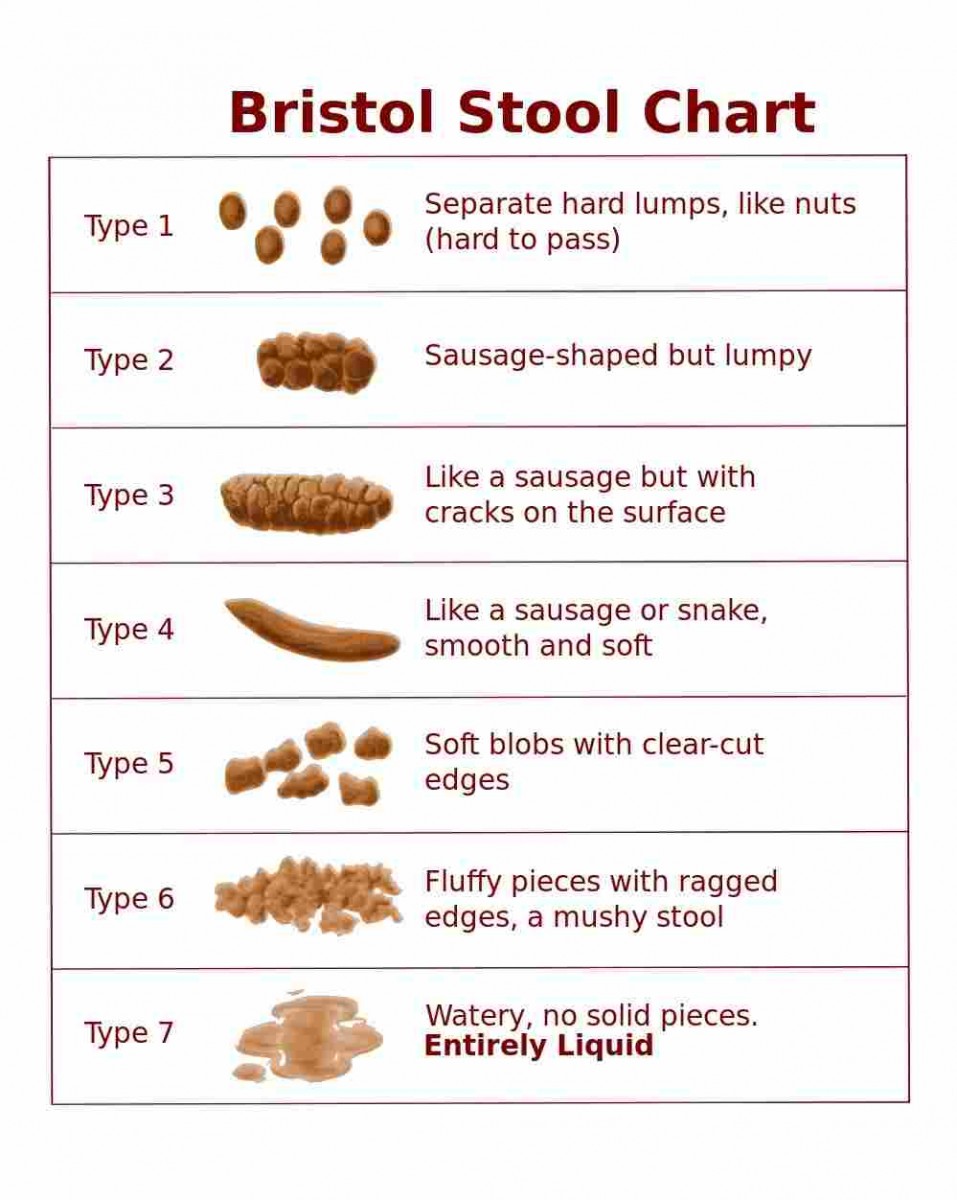
Constipation is the passage of less than three bowel movements in a week.
Common signs of constipation include;
- Stools that are dry, hard, lumpy
- Stools that are difficult or painful to pass
- A feeling that you have not completely emptied your bowel
The Bristol Stool Chart is a recognised pictorial diagram used in healthcare that you can use to classify your stools. Type 1 and type 2 indicate constipation.
Why might I become constipated?
Factors that could be contributing to changes to your bowel habits include;
- Irregular eating pattern
- Eating less than you usually would
- Changes to your diet i.e. fibre content, texture/consistency
- Drinking less fluid
- Reduced activity level
- Medications i.e. opioid-based pain medication such as; morphine, codeine; diuretics (water tablets) such as furosemide
How can I manage constipation?
Making small changes to your fluid intake, fibre intake and activity level can change the form of your stool to make it easier for your body to push waste along your digestive tract.
Drink more fluid
 Aim to drink at least 6-8 mugs of fluid per day. This will soften your stool and make it easier to pass.
Aim to drink at least 6-8 mugs of fluid per day. This will soften your stool and make it easier to pass.
Water, tea, coffee, milk, yoghurt drinks, diluting juice, fruit juice, soda, fizzy juice, soups and beef stock all count.
Alcohol does not count towards your fluid intake and can increase risk of dehydration so it is best to limit or avoid alcohol if you are constipated.
Keep a check on the colour of your urine. This is a good indicator of whether or not you are drinking enough. If you are drinking enough, your urine will be pale or straw coloured. If your urine is dark, you will need to drink more to avoid dehydration.
Tips to help increase your fluid intake
- Use a straw
- Try a variety of different drinks
- Use a larger drinking cup or glass or choose one with handles
- Keep a drink within reach at all times throughout the day
- Try using a water bottle to help you measure how much you are drinking
- If you are going out, take a drink with you
Eat more fibre
 As part of a healthy balanced diet the general population is encouraged to eat 30g fibre per day. This can be difficult to achieve particularly if you have a poor appetite.
As part of a healthy balanced diet the general population is encouraged to eat 30g fibre per day. This can be difficult to achieve particularly if you have a poor appetite.
Foods with a higher fibre content can make you feel full and tend to have less calories in them. If you have a small appetite or are trying to gain weight this may not be practical.
If you are adding fibre to your diet do it gradually introducing 1-2 changes every few days. This will help your bowel adjust and avoid bloating and excess gas.
Fibre absorbs fluid. You may need to drink more if you increase the fibre content of your diet to avoid worsening your symptoms.
For more information on how to include fibre in your diet visit The British Dietetic Association or The British Nutrition Foundation.
As a starting point see below for examples of higher and lower fibre containing foods. Try choosing a higher fibre alternative;
Higher fibre alternative |
Lower fibre alternative |
| Seeded or wholemeal bread or bread products, pitta, wraps, roti, rye | White bread, white rolls, white pitta bread, white wrap, crumpet, pancake |
| Oatcakes, crispbread, rice cakes, popcorn | Cream crackers, breadsticks, rice cakes, crisps, biscuits |
|
Bran flakes, porridge oats, muesli, wholegrain cereal Tip: mix your regular cereal with a higher fibre alternative to introduce the fibre gradually |
Refined breakfast cereals i.e. corn or rice based cereals |
| Wholemeal pasta, quinoa, bulgar wheat, brown rice, millet, rye, barley, maize, wholewheat noodles | White pasta, white rice, basmati rice, noodles |
| Baked potato or boiled potato (skin on), sweet potato or yam | Mashed potato/boiled or baked potato (skin off) |
| Nuts, seeds | Ground nuts |
| Lentils, kidney beans, yellow-split peas, baked beans, chickpeas | Skinned chicken, white fish, hard boiled egg |
| Orange, satsuma, apple, kiwi fruit with seeds, watermelon, pineapple, dried apricots, raisins, prunes | Skinless or tinned fruit i.e. apple, peach, pear, galia melon, banana |
| Raw vegetables, peas, sweetcorn | Well-cooked or skinless fruit and vegetables i.e. carrot, broccoli or grated veg |
Increasing the fibre content of your diet may not be suitable for everyone, particularly if you have a stoma, cancer affecting the digestive tract including stomach, bowel/colon or have been advised that you are at risk of developing a bowel obstruction.
What if I have a stoma?
The information on this page is not suitable for you if you have a stoma. Speak to your healthcare team if you are looking for advice specific to eating and drinking with a stoma.
What if I have a stent?
The information on this page is not suitable for you if you have a stent anywhere along your digestive tract. Speak to your healthcare team if you are looking for advice specific to eating and drinking with a stent in this area.
Increase your activity level
 You will benefit from any increase in exercise.
You will benefit from any increase in exercise.
Try a short walk, chair exercises, household chores such as dusting, gardening, hoovering or choose to take the stairs instead of the lift.
Try to limit time spent watching television or using other devices to encourage you to move around more.
For more information on introducing activity visit NHS Inform or Macmillan Cancer Support.
What about medication?
 Laxatives are a medication that can help with constipation and encourage you to pass a bowel movement.
Laxatives are a medication that can help with constipation and encourage you to pass a bowel movement.
If you have been prescribed laxatives you should continue to take these. If you do not think these are helping your symptoms please discuss this with your pharmacist or a healthcare professional. There are many types of laxatives that work in different ways. Your dose or type of medication may need altered.
If you are not prescribed any medication to help treat your constipation and you think this could help you please discuss this with a healthcare professional.
What if I have an ileostomy or a colostomy?
The information on this page is not suitable for you if you have a stoma. Speak to your healthcare team if you need advice specific to eating and drinking with a stoma.
