

Prehabilitation - Getting Ready for Cancer Care






Prehabilitation - Getting Ready for Cancer Care
What is Prehabilitation?
The North Cancer Alliance has been running a programme since August 2021 called ‘Transforming Cancer Care’ funded by Macmillan and the Scottish Government to enhance the lives of people with cancer. A key piece of work that has been progressing is around a concept called ‘prehabilitation’. This is used to describe the things people can do, or be supported with to get ready for cancer treatment or surgery. There is a growing body of evidence to suggest that physical activity or movement, good mental health and good nutrition before treatment or surgery can help quicker recovery and better resilience.
Macmillan developed this model in the past few years, working with the Royal College of Anaesthetists and the National Institute of Health Research (NIHR) Principles and guidance for prehabilitation within the management and support of people with cancer (Macmillan.org.uk)
So, prehabilitation activity seeks to get people fit for their surgery/treatment, which is hoped will improve outcomes for people. However, prehabilitation should not in itself mean patients wait longer for their surgery or treatment, but it does make best use of the time people have before they get their start/surgery date.
What are the different parts of Prehabilitation?
Prehabilitation is like looking at a table split into 12 parts.
Looking at the left hand column we have the different aspects or ‘modalities’ of prehabilitation. These are what has already been mentioned; physical activity, good nutrition or diet and good mental wellbeing. There is a fourth, around healthy lifestyle, which means thinking about changing smoking, alcohol and substance consumption.

Looking at the top row we have 3 levels. They reflect levels of need for each modality. So, for example, a healthy 55 year old man is diagnosed with early stage colorectal cancer. The team in the hospital have agreed that he needs an operation (surgery) to get out the tumour and surrounding lymph nodes. He walks regularly and his diet is mostly OK. He is shocked by the diagnosis, but he is still able to look on the positive side and he has a supportive partner to help him. Expressed in green below, he requires ‘universal’ prehab which means a light touch support, maybe some general advice on diet and to continue the walking till the day of surgery, and a listening ear to help him process the diagnosis.
However, for a 65 year old woman, a smoker who may also have Type 2 Diabetes and be overweight. Then she gets diagnosis of ovarian cancer - which itself is a more complex condition. This lady may require a higher level of support from a number of professionals during her prehabilitation. She faces more risks from her surgery and/or treatment due to her being overweight and her long term conditions, so more monitoring and care is needed, especially around diet and exercise. Her diagnosis may also impact her mental health and require a higher level of emotional support. Her prehabilitation needs are expressed in the table in pink.
Who is Prehabilitation For?
Prehabilitation can benefit anyone who is preparing for cancer treatment, be it chemotherapy, radiotherapy, immunotherapy or other kind of treatment, as well as surgery. It is also beneficial for patients who are receiving palliative care as well as those who are being treated with the intent to cure the cancer.

Why is Prehabilitation Important?
Key benefits for patients are feeling more in control of their lives and a sense that they are contributing to better outcomes for their cancer surgery or treatment. There is also evidence to suggest that recovery is quicker following surgery and during/after treatment if prehabilitation is followed. The Table below demonstrates the predicted pathway of health with and without prehabilitation, with better outcomes for those who optimise their fitness before treatment (or surgery).
Prehabilitation can also kick-start a healthier lifestyle after cancer, maybe with exercise, healthy eating and self-caring for emotional well-being carrying on, to help people stay healthy and strong over the longer term. 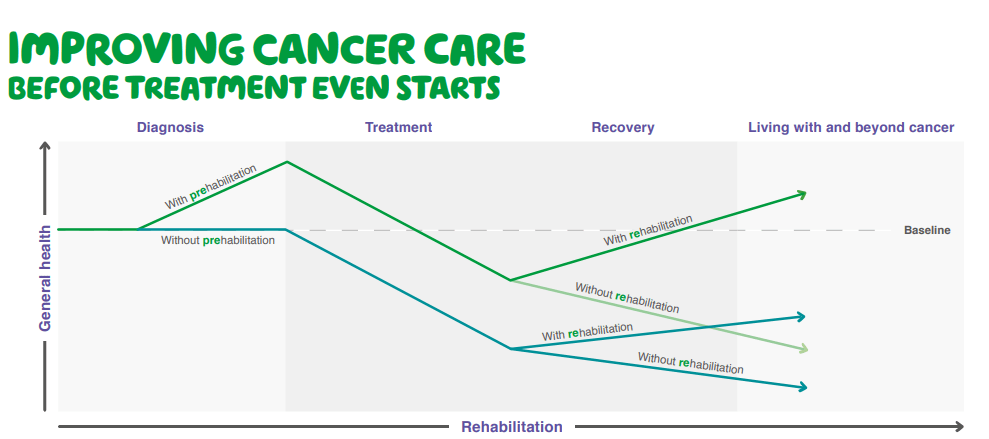
What have we been doing in Scotland?
The Scottish Government has worked with clinicians, NHS cancer alliances and the third sector to develop national principles of prehabilitation. The North Cancer Alliance has been part of this work.
Prehabilitation for Scotland - Small changes make a big difference (nhs.scot)
They have also developed Frameworks for psychological support and nutritional support
Psychological Framework – Prehabilitation for Scotland (nhs.scot)
Nutrition Framework – Prehabilitation for Scotland (nhs.scot)
The principles and frameworks offer information on what patients should have access to and when, to help them do prehabilitation effectively and to set patients up for healthier lives after their treatment or surgery or after their cancer journey.
What about Prehabilitation for the North of Scotland (Tayside, Grampian, Highland, Shetland, Orkney and the Western Isles)?
Prehabilitation is still a new concept for many in NHS cancer care and among the community at large. For many years, the focus has been on the treatment and surgery itself, followed by the rehabilitation afterwards. However, the idea of ‘getting ready’ for cancer care is one that many patients are welcoming, particularly those who didn’t do prehab but wished they had come in to their treatment or surgery fitter and stronger. “You wouldn’t run a marathon without training, and this is the same thing.”
The prehabilitation programme in the North has focused on a community approach, to find out about the potential of community assets – things like local walking groups, leisure centre classes and charity services, to be part of prehabilitation provision, alongside the formal hospital services. Core to the regional work has also been to consider the rurality and remoteness of our area and what this means for providing equal and sustainable access to prehabilitation for our people. We know that some people face long journeys for diagnostic tests and for surgery and treatment, which may involve more than one ferry trip and maybe a journey by air. We also know that we can’t always provide services digitally, so creative solutions are sometimes needed.
The work is overseen by a Steering Group that is led by Meghan McEwen who is Chair of NHS Orkney. The group includes a number of NHS staff and providers of cancer support from the third sector, such as Maggies, CLAN and Macmillan. Scoping something as big as prehabilitation across a whole region is gradual work and the pressures on the NHS since 2020 has created barriers, as well as opportunities for the project to develop. Here are the things we have achieved since August 2021
- The Programme has identified an encouraging level of buy-in for the ideas around prehabilitation for the benefit of patient groups in the longer term. Progress has also been made in locating and collaborating with tests of change across the North, including Island boards. We have also developed some great relationships with cancer charities for the future.
- We have developed and launched a North of Scotland Nutrition information webpage to support patients to access high-quality dietetic advice.
- The project has set up a patient and carer reference group, which has been vital in providing lived experience of ‘walking along’ pathways. We have also developed valuable relationships with Board Public Involvement Teams and with HIS-Engage Outreach.
- The project has identified a number of ‘way finders’ across local areas that can support patients (and staff) to direct them to suitable community assets which could provide prehabilitation input. We have also identified a large number of local community level activities and supports for our patient groups and digital assets they may want to use. We will soon be adding more information about who can help with prehabilitation in your area.
What’s Happening Next?
There is still work to do to make it a ‘standard’ or ‘opt out’ activity but prehabilitation is gaining traction around Scotland and the UK because of the benefits it can create.
We have identified some priorities for the next two years around:
- Creating a ‘community of practice’ of prehabilitation practitioners and patients to share learning more widely and to create more interest in the concepts of prehabilitation.
- Supporting specific communities to access prehab that may otherwise face barriers, including rurality, the cost of living pressures and health inequalities.
- We have also identified a really exciting test of change for more complex prehabilitation to happen within head and neck cancer services.
